
Cardiomyopathy and Stroke Risk: What You Need to Know
When you’re managing a heart condition like cardiomyopathy, the focus is often on the heart itself. However, being diagnosed with this condition can also bring an increased risk of other health complications—many of which can be well controlled with the right care and attention.
One of the most significant risks is stroke. In fact, according to the American Heart Association, someone in the United States has a stroke every 40 seconds, which shows how common and urgent this condition is.
Why understanding it matters:
- Stroke is the 5th leading cause of death in the U.S.
- People with heart conditions, like cardiomyopathy, face higher risk.
- Quick action saves lives and reduces long-term damage.
In this article, we’ll explain how cardiomyopathy can increase stroke risk, what signs to watch for, and the steps you can take to stay protected.
Understanding Cardiomyopathy
Cardiomyopathy is a heart condition that affects the muscle’s ability to pump blood effectively. Understanding the different types of cardiomyopathy can help you and your care team determine your specific risks and the best ways to manage them:
- Hypertrophic cardiomyopathy (HCM): Thickened heart muscle that can obstruct blood flow and trigger rhythm problems.
- Dilated cardiomyopathy (DCM): Enlarged and weakened heart chambers, reducing pumping power.
All of these types of cardiomyopathy share a common challenge—they put extra strain on your heart, making it harder for blood to flow normally and increasing the risk of blood clots and stroke.
What Is Stroke?
A stroke happens when the blood supply to part of the brain is suddenly interrupted, preventing oxygen and nutrients from reaching brain cells. Within minutes, this lack of oxygen can start damaging brain tissue, which is why stroke is such a medical emergency.
There are two main ways a stroke can happen:
- Ischemic stroke: The most common type, caused by a blood clot blocking an artery in the brain.
- Hemorrhagic stroke: Caused by bleeding in or around the brain when a blood vessel bursts.
You might have heard your doctor mention “clot-related stroke” if you have cardiomyopathy. This refers to an ischemic stroke. According to the American Heart Association, about 87% of all strokes are ischemic. This means they’re caused by a clot blocking blood flow to the brain, which aligns with the increased clotting risk in cardiomyopathy.
The Stroke Connection: How Cardiomyopathy Affects Stroke Risk
People with cardiomyopathy face a higher risk of stroke because changes in the heart’s rhythm and structure can make it easier for blood clots to form.
This increased risk comes down to a few key ways cardiomyopathy can affect the heart:
- Atrial Fibrillation (AFib): In many people with HCM and some other types, the heart’s upper chambers (the atria) can start to beat irregularly. This irregular rhythm makes it harder for blood to flow smoothly, allowing it to pool and form clots—which can then travel to the brain.
- Weakened Pumping Ability: In DCM, the heart muscle becomes stretched and weakened. When the heart can’t pump strongly, blood can slow down and stagnate inside the chambers, creating a higher chance for clots to develop.
- Structural Heart Changes: When the heart walls become thickened or enlarged (common in several types of cardiomyopathy), they create spaces or pockets where blood may sit longer than it should. These small clots can break loose, travel through your bloodstream, and block an artery in the brain (known as a cardioembolic stroke).
Managing Stroke Risk When You Have Cardiomyopathy
If you’re living with cardiomyopathy, whether DCM, HCM, or another type, it’s reassuring to know that while stroke risk can be higher, there are clear steps you and your care team can take to manage it more effectively.
Here’s what to keep in mind:
- Know Your Personal Risk: Not everyone with cardiomyopathy has the same risk of stroke. Your risk depends on factors like the type of cardiomyopathy you have, whether you also have AFib, and how well your heart is pumping. Regular check-ups and monitoring—such as echocardiograms or Holter monitors—help your doctor assess your individual risk.
- Watch for Symptoms: Being aware of stroke symptoms—like sudden weakness, trouble speaking, or vision changes—means you can act quickly if something feels wrong. Early treatment can greatly improve outcomes.
- Follow Your Treatment Plan: Your doctor may recommend medications like blood thinners if your risk is high, especially if AFib is present. Managing blood pressure, keeping a heart-healthy lifestyle, and staying on top of your appointments all play a role in reducing stroke risk.
- Ask About Monitoring Options: Technology, like wearable devices, can provide continuous insights into your heart’s rhythm, helping catch any changes early. Discuss with your care team whether continuous monitoring might be helpful for you.
Recognizing Stroke: Key Signs to Act On
Knowing the signs of a stroke, and acting fast, can make a life-changing difference. Stroke symptoms can come on suddenly and may vary from person to person, but certain warning signs are important to recognize right away:
- Weakness or numbness, especially on one side of the body
- Trouble speaking or understanding
- Vision loss in one or both eyes
- Dizziness or loss of balance
- A sudden, severe headache with no clear cause
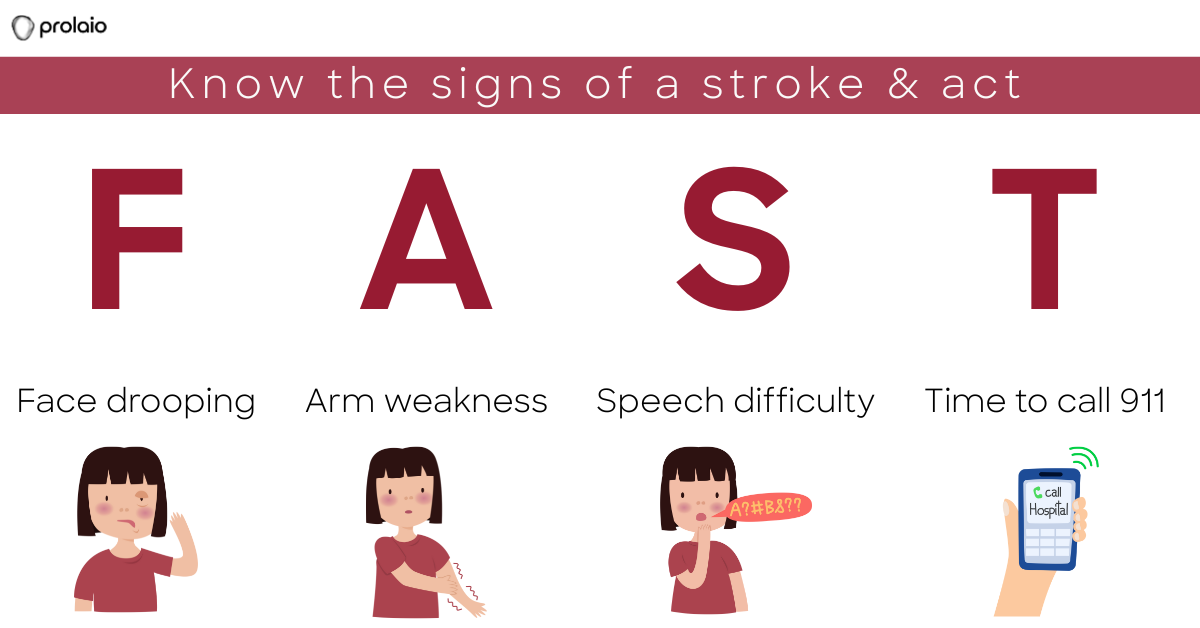
Remember F.A.S.T.:
Quick action can make a big difference in recovery. According to the American Stroke Association, patients who receive clot-busting treatment (like tPA) within 3 hours of symptom onset are 30% more likely to recover with little or no disability.
Take Control of Your Health
Learning that cardiomyopathy increases stroke risk can feel overwhelming—but with the right knowledge and a clear care plan, you can take meaningful steps to stay protected. Regular monitoring, following your care team’s guidance, and staying alert to new or changing symptoms are key. Proactive care truly makes all the difference.
Learn how Prolaio’s around-the-clock heart monitoring aims to help you and your care team track how your heart responds to treatment and catch early warning signs—before complications arise.
Join our community for real stories, new research, and everyday tips to help manage cardiomyopathy.
Disclosure
*This content is for informational purposes only and should not be taken as medical advice. Always consult your healthcare team for guidance specific to your condition.*
References
Tsao CW, Aday AW, Almarzooq ZI, and others. Heart disease and stroke statistics—2023 update, a report from the American Heart Association. Published in Circulation, February 2023.